Discover the causes, symptoms, and treatments for Interstitial Cystitis to manage chronic bladder pain and improve quality of life.
Over 3 million Americans are estimated to live with chronic bladder pain due to Interstitial Cystitis—a condition that can deeply impact everyday life. This comprehensive guide is designed to empower you with essential insights about interstitial cystitis, from its causes and symptoms to effective treatments and lifestyle adjustments. We understand how overwhelming it can be to face the challenges of interstitial cystitis, but you’re not alone. In the next few minutes, you’ll gain valuable knowledge to take control of your health journey. Let’s take the first step together toward a healthier, happier future!
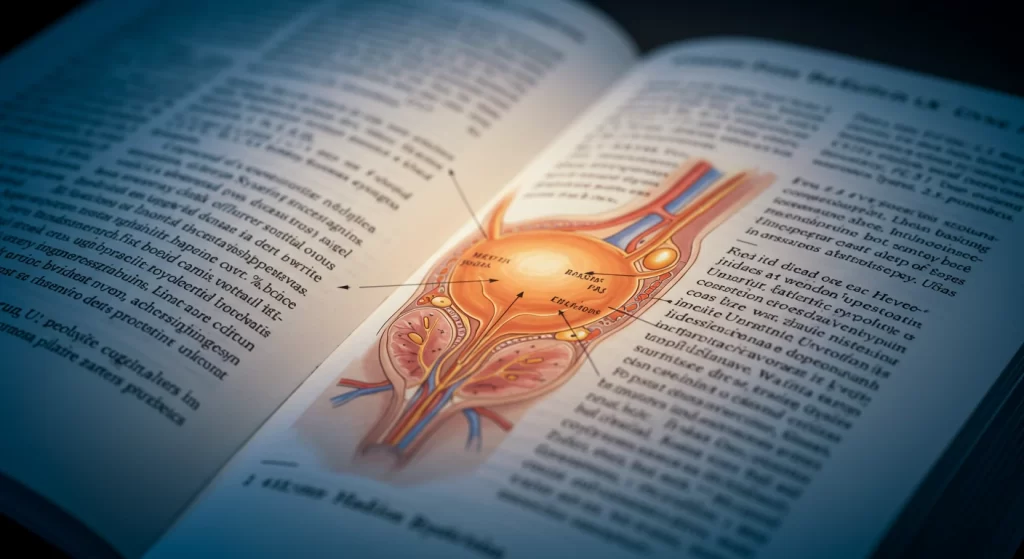
Causes and Risk Factors of Interstitial Cystitis
Understanding the root causes of Interstitial Cystitis is key to managing its symptoms. Although its exact origin remains unclear, several risk factors and potential triggers have been identified:
- Genetic predisposition: A family history of bladder issues can increase the likelihood of developing interstitial cystitis.
- Autoimmune responses: Some experts believe the body’s immune system may mistakenly attack bladder tissues.
- Hormonal influences: Women, particularly those in their reproductive years, are more susceptible.
- Environmental triggers: Certain foods, stress, or infections may exacerbate the condition.
- Physical factors: Past bladder injuries or surgeries may also contribute.
By recognizing these risk factors early, patients can work with their healthcare providers to develop proactive management strategies.
Common Symptoms Women Should Recognize
Interstitial cystitis presents with a variety of symptoms that may vary from person to person. Being aware of these early signs can lead to timely intervention:
- Chronic pelvic pain: Often the most debilitating symptom, ranging from mild discomfort to severe pain.
- Frequent urination: An increased urge to urinate, sometimes up to 60 times a day.
- Urgency: A persistent need to void immediately, even if only small amounts of urine are produced.
- Pressure or tenderness: Sensations of fullness or pressure in the bladder area.
- Pain during intercourse: Discomfort that can affect intimate relationships and overall well-being.
If you experience any of these symptoms persistently, consult a healthcare professional. Early diagnosis is crucial in managing interstitial cystitis effectively.
How Interstitial Cystitis Affects Daily Life
Living with Interstitial Cystitis can be challenging, as the condition often interferes with everyday activities and quality of life. The constant discomfort and frequent bathroom trips can impact work, social interactions, and mental health. Many patients report:
- Social isolation: Due to the unpredictable nature of symptoms, some individuals avoid outings or social gatherings.
- Emotional distress: Chronic pain and uncertainty can lead to anxiety, depression, and a sense of loss over one’s previous lifestyle.
- Work limitations: Frequent absences or reduced productivity may occur as managing symptoms takes priority.
- Sleep disturbances: Nocturia (frequent urination at night) often disrupts sleep, leading to fatigue and reduced daytime performance.
Despite these challenges, understanding the impact of interstitial cystitis on your daily routine is the first step toward regaining control and implementing effective coping strategies.
Available Treatments and Pain Management
The treatment landscape for Interstitial Cystitis is as diverse as its symptoms. No single approach fits every patient, so treatment plans are often personalized. Some common strategies include:
- Medications: Oral medications like pentosan polysulfate sodium (PPS) help repair the bladder lining, while pain relievers and anti-inflammatory drugs can ease discomfort.
- Bladder instillations: Directly administering medication into the bladder may provide relief from pain and urgency.
- Physical therapy: Specialized pelvic floor therapy can reduce muscle spasms and improve bladder control.
- Behavioral modifications: Techniques such as timed voiding and stress management are crucial in reducing symptom flare-ups.
- Alternative therapies: Acupuncture, dietary supplements, and biofeedback have shown promise in some cases.
Working closely with a healthcare provider will help determine the best combination of treatments for your specific situation. With a multifaceted approach, it is possible to significantly reduce pain and improve quality of life.
Dietary Changes to Reduce Bladder Irritation
Diet plays a critical role in managing Interstitial Cystitis. Certain foods and beverages can irritate the bladder, worsening symptoms. Consider these dietary modifications:
- Avoid trigger foods: Common culprits include caffeine, alcohol, citrus fruits, spicy foods, and artificial sweeteners.
- Increase water intake: Staying well-hydrated helps dilute irritants and flush the bladder.
- Incorporate anti-inflammatory foods: Omega-3 fatty acids, found in fish and flaxseeds, and antioxidants from leafy greens can help reduce inflammation.
- Experiment with an elimination diet: Identify and remove potential triggers, then slowly reintroduce them to determine tolerance.
A well-balanced, bladder-friendly diet can make a significant difference in managing interstitial cystitis. Keeping a food diary may help you identify which foods exacerbate your symptoms.
New Research and Future Treatment Options
Emerging research is continuously broadening our understanding of Interstitial Cystitis. Scientists are investigating several promising areas:
- Stem cell therapy: Early studies suggest potential in regenerating damaged bladder tissue.
- Novel drug therapies: Researchers are exploring new medications that target the underlying causes of bladder inflammation.
- Genetic studies: Understanding genetic factors may lead to personalized treatments tailored to individual risk profiles.
- Microbiome research: The role of gut and urinary microbiota in inflammation is an exciting new frontier.
These advances offer hope for more effective treatments and, eventually, a cure. Staying informed about the latest developments empowers you to advocate for cutting-edge care and participate in clinical trials if appropriate.
FAQs
Q: What are the main causes of Interstitial Cystitis?
A: The exact cause of interstitial cystitis is unknown, but it’s believed to involve a combination of genetic, autoimmune, and environmental factors.
Q: How can I prevent complications from Interstitial Cystitis?
A: Early detection through routine screenings, avoiding dietary triggers, and working closely with your healthcare provider can help manage symptoms and prevent complications.
Q: When should I seek help for Interstitial Cystitis?
A: If you experience persistent pelvic pain, frequent urination, or other related symptoms, it’s important to consult a doctor as soon as possible.

Conclusion
Every step you take toward understanding and managing Interstitial Cystitis is a victory worth celebrating. With early detection, proactive dietary changes, and personalized treatment plans, you can reduce chronic bladder pain and reclaim your quality of life. Remember, you have the power to create lasting change! Share this guide with someone who might benefit from it, or reach out to a trusted healthcare professional for personalized advice. Together, we can build a healthier tomorrow.
If you’re struggling with interstitial cystitis, know that help is available. Consider joining support groups or consulting experts who can offer guidance—you deserve support and care.

